Alternative treatments to spinal fusion
/ Targeted Conditions
What is spinal fusion?
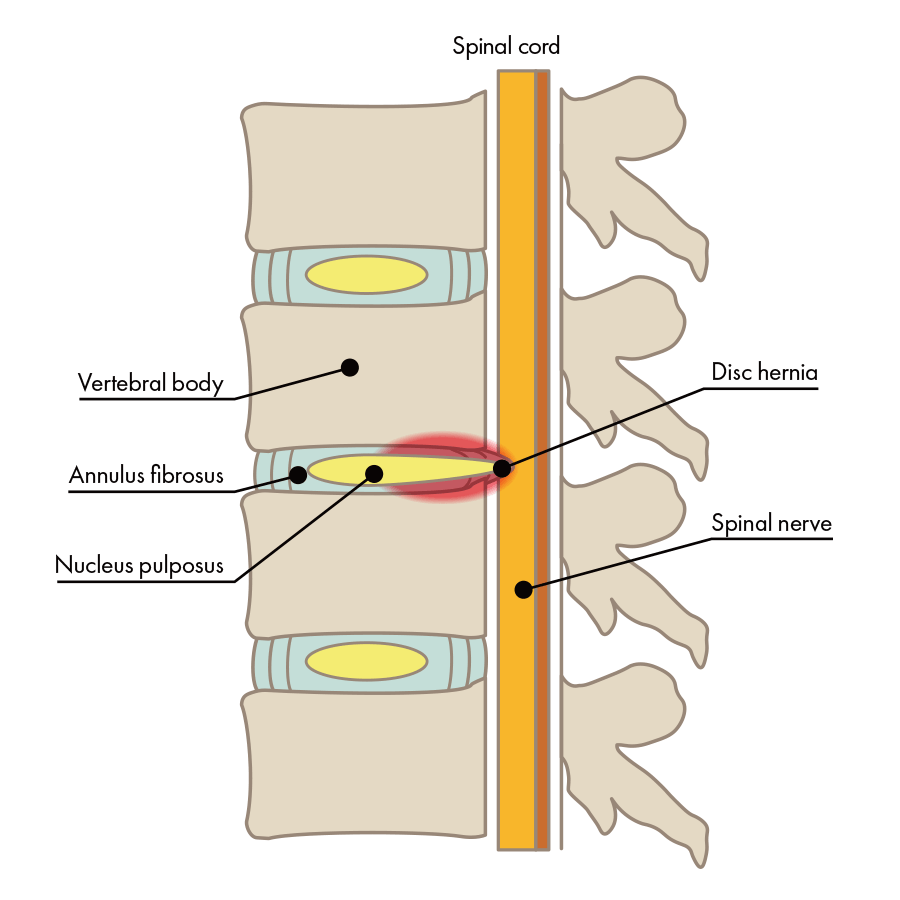
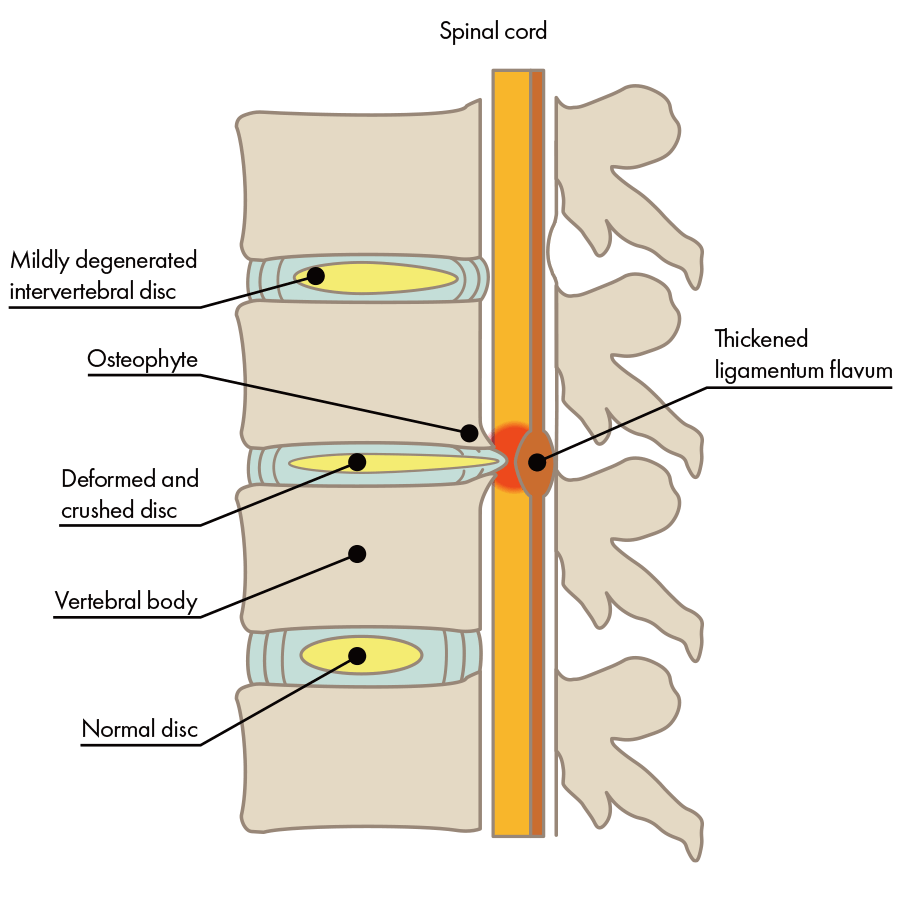
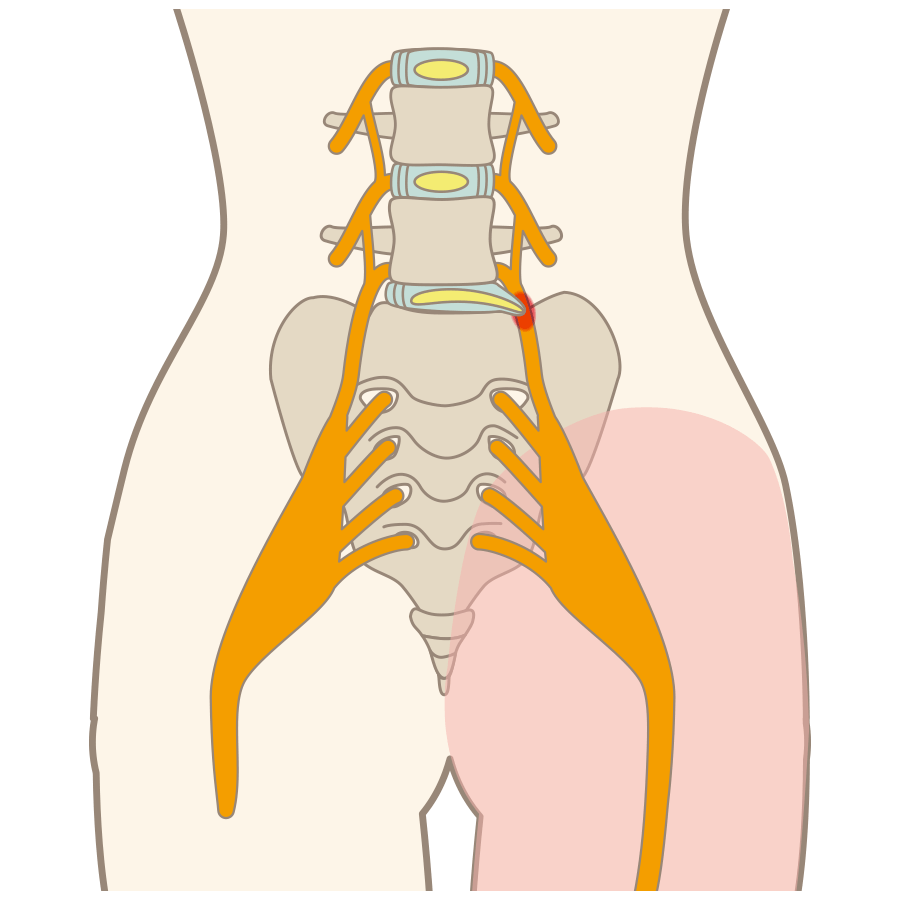
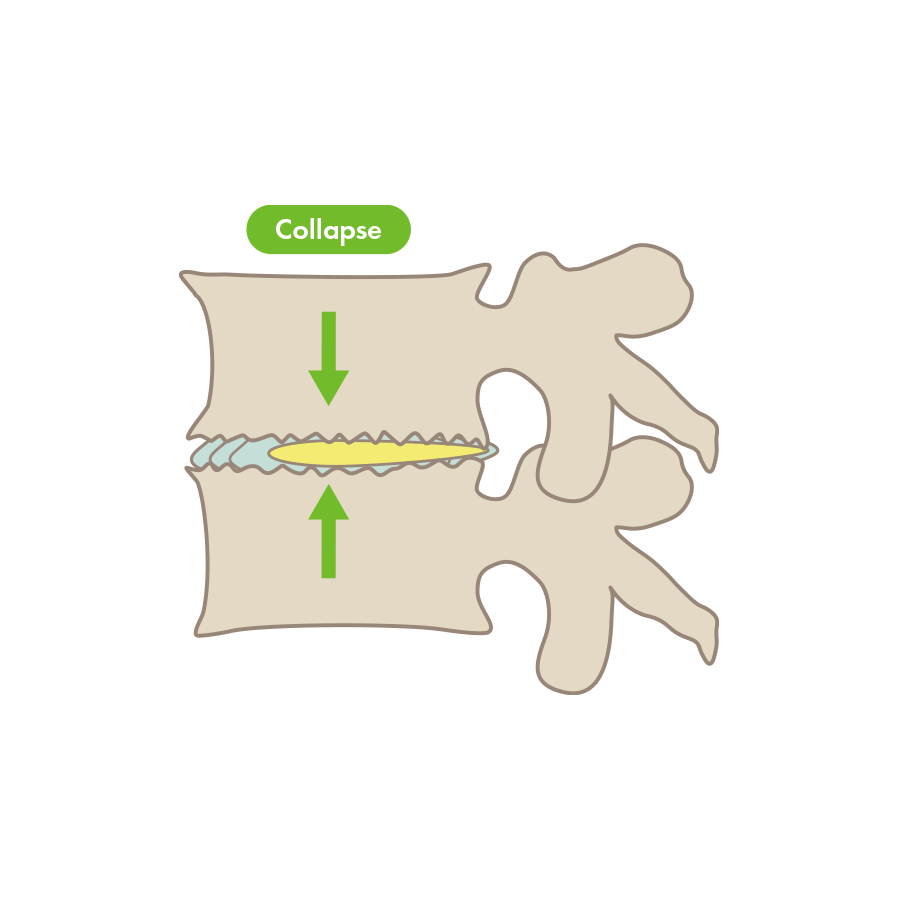
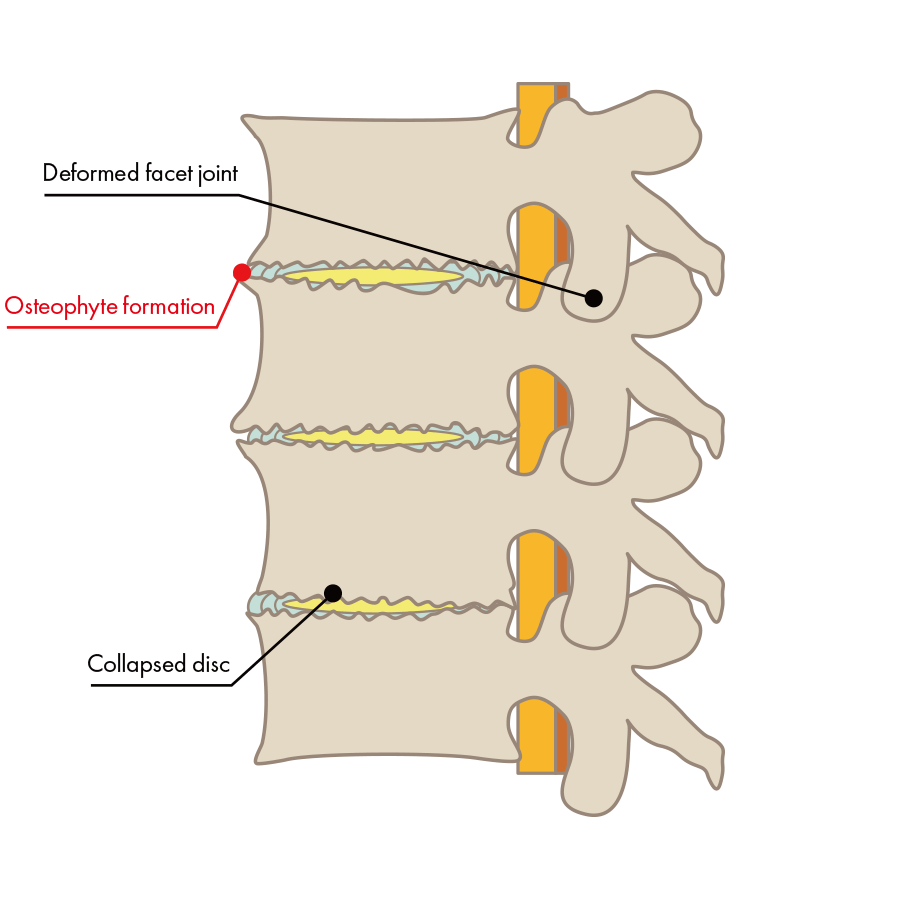
Spinal fusion is a surgical procedure of the spine that uses plates, screws, rods and spacers to fix together adjacent vertebrae. It is performed in case of back pain related disorders such as lumbar disc herniation, spinal canal stenosis, spondylolisthesis, degenerative spondylolisthesis, etc., which are caused by imbalance of the spine as a result of aging or heavy labor. When a nerve root is compressed, severe back pain and numbness in the back and legs may appear when walking. The procedure is used to decompress the nerve and relieve symptoms.
Spinal Fusion Techniques
Posterior Lumbar Fusion
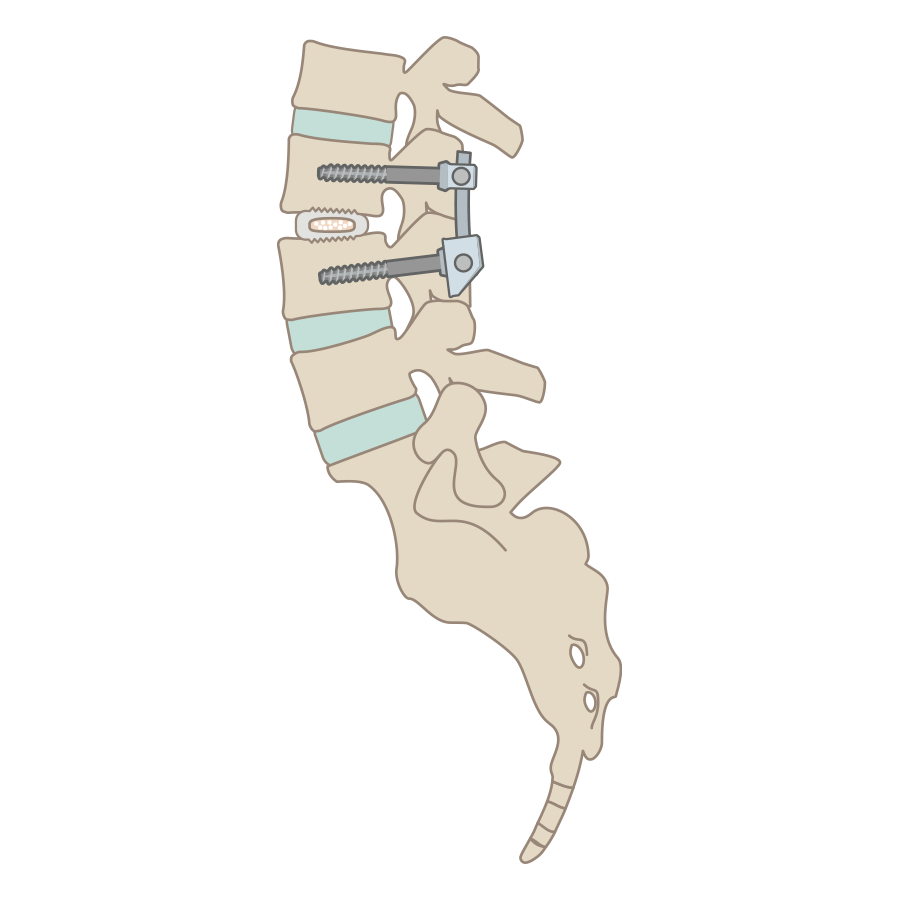
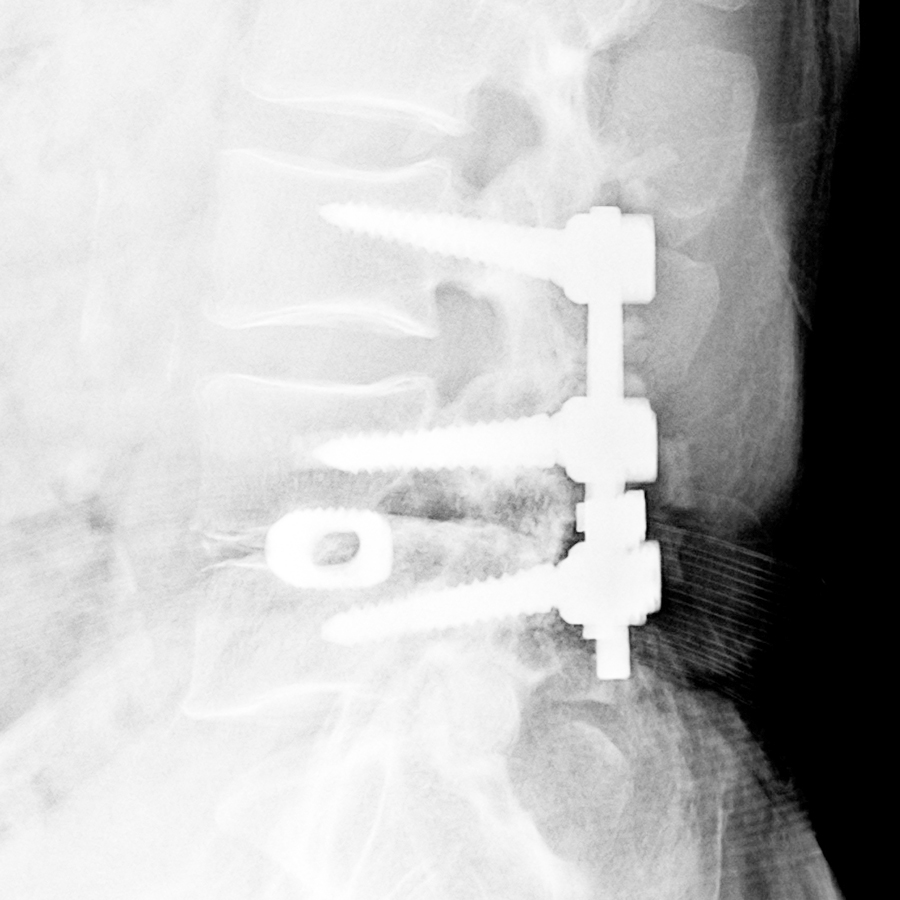
This is a surgical method to hold the vertebrae together that is performed from the posterior side of the back. Access from the posterior side is often preferred when treating lumbar spinal canal stenosis, lumbar disc herniation, lumbar spondylolisthesis, lumbar spondylolisthesis, and lumbar degenerative spondylolisthesis. First, it involves removing a part of the vertebrae called the vertebral arch and the spinous process from the lumbar vertebrae, as well as the intervertebral discs and ligamentum flavum. Next a spacer is inserted in place of the intervertebral disc between the upper and lower vertebrae so as not to damage the nerve, and a metal plate is set on the vertebral bodies and secured by means of rods and screws.
Posterior Lateral Lumbar Fusion
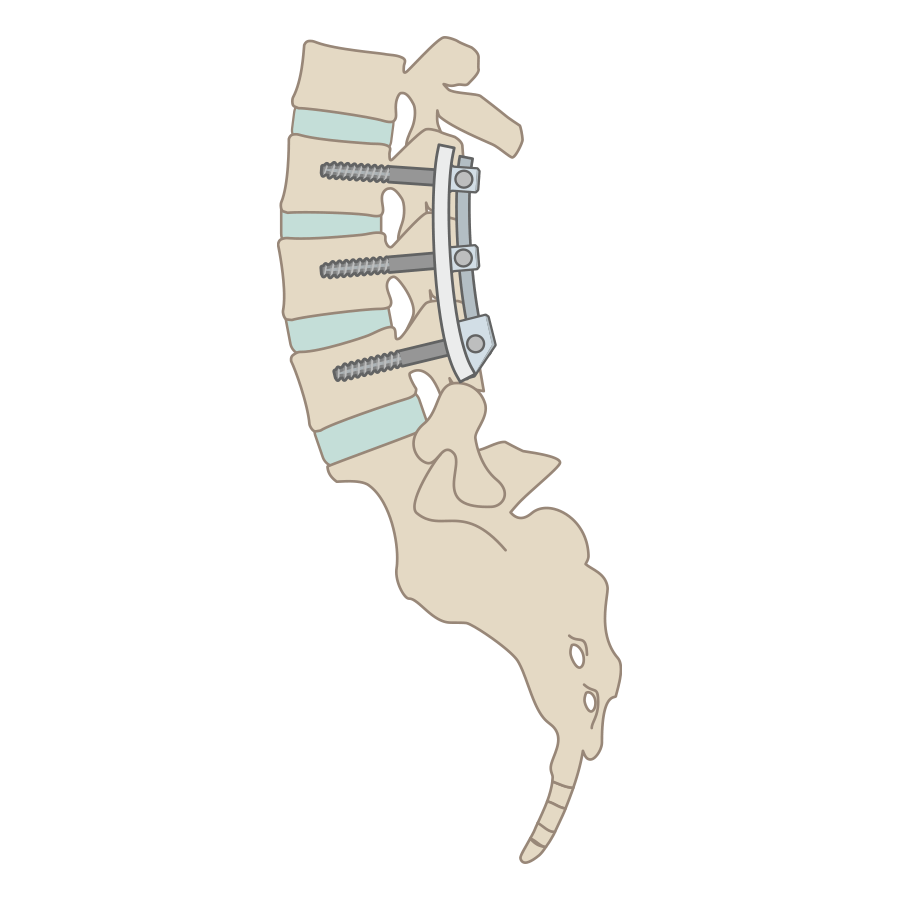
This is a surgical procedure similar to the posterior vertebral fusion that fuses vertebral bodies from the backbone. The posterior vertebral arch is removed, and the posterior vertebrae are held together using the patient's own bone material as well as metal devices to prevent injury to the nerve. This method does not involve the removal of the disc or ligamentum flavum.
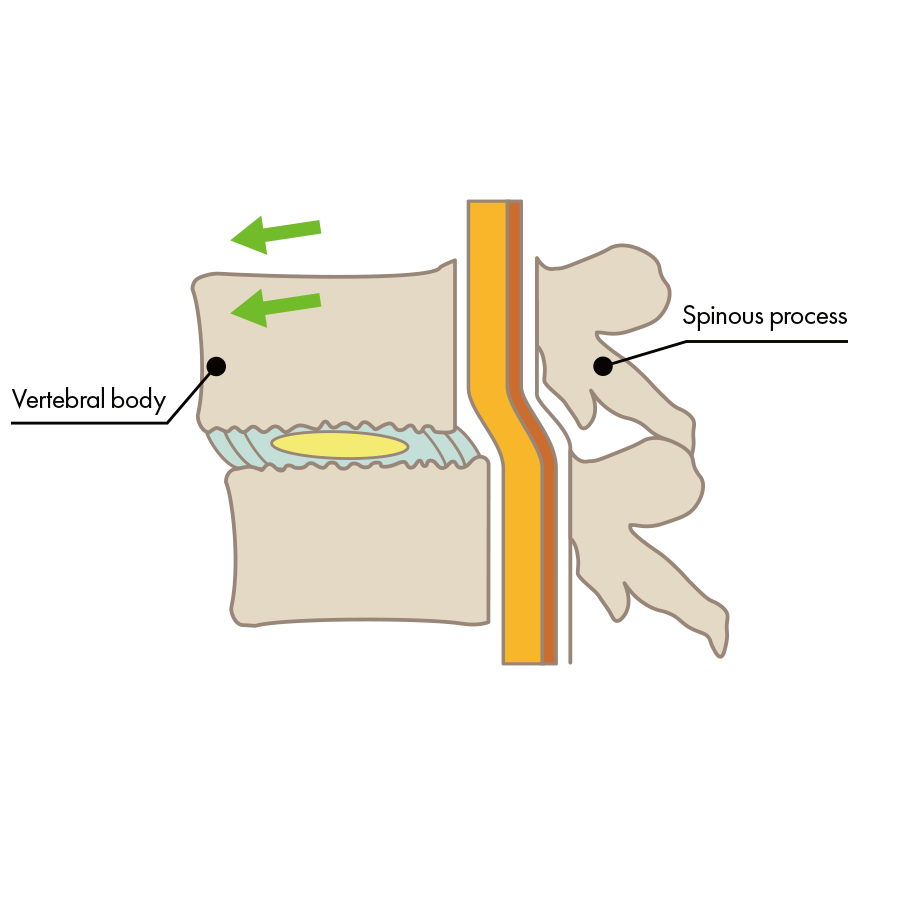
Anterior Lumbar Fusion
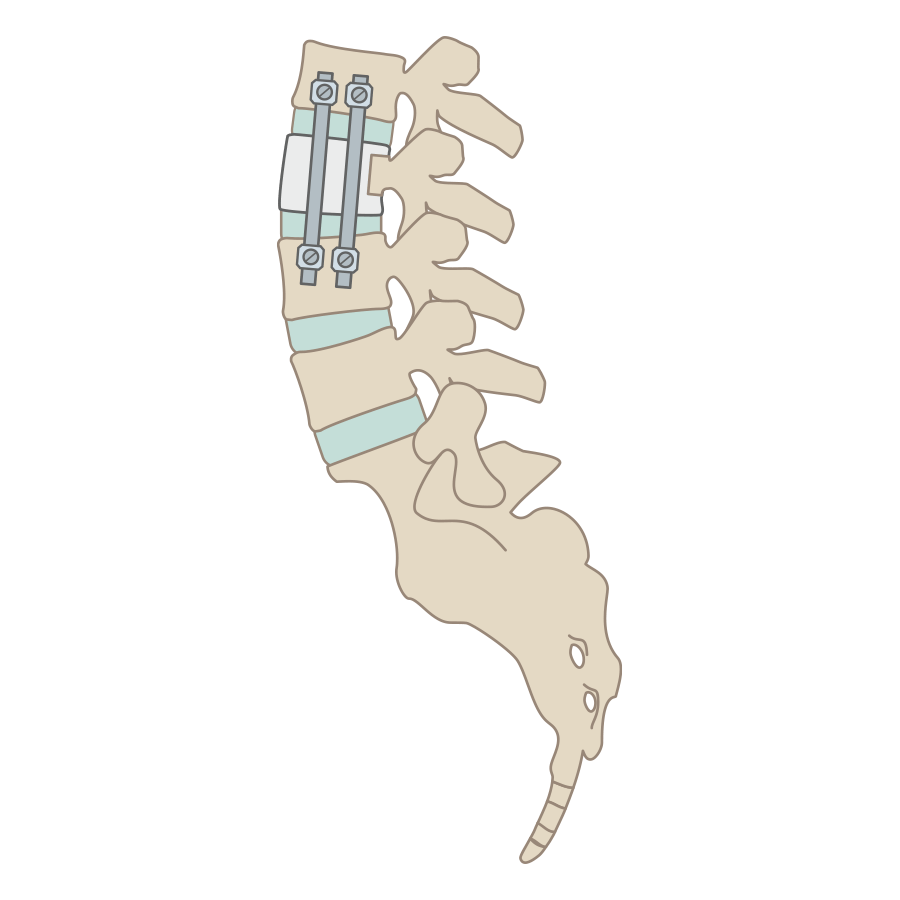
This surgical procedure is performed when vertebrae in the lower back (the spine) have been fractured. During the anterior vertebral fusion, an incision is made from the side of the abdomen, and the intervertebral discs around the fractured vertebrae and the remnants of vertebral bodies are removed. The patient's own bone matter (bone graft) or bonelike material is used to replace the vertebrae or intervertebral discs and are held in place using fixation devices.
It is said that these techniques, by creating a space between the spinal canal and the nerve, can relieve the pressure on the nerve that is the cause of pain and numbness. However, in the event of a surgical procedure, the relapse rate is said to be generally around 30 to 45% (*1), and depending on the physical condition of the patient, the surgery itself may pose a risk. On some occasions, the patients may not be permitted to have surgery even if they wish to undergo it.
Spinal fusion is not always indicated in case of lumbar disc herniation, lumbar spinal canal stenosis, lumbar spondylolisthesis, lumbar degenerative spondylolisthesis, etc. There are also conservative medication treatment, endoscopic surgical treatments,etc. , and it is recommended that you consult your clinic or hospital to see if spinal fusion is indicated.
Postoperative pain and rehabilitation after spinal fusion
After spinal fusion surgery, patients may feel pain due to the inserted fixation device. Although there are individual differences, some patients may experience symptoms such as discomfort, fatigue, and pain in their lower back for up to a year. Even if the surgery is performed without any problem, the original pain and numbness may recur, so it is necessary to be aware of the pain and risks after spinal fusion surgery in advance.
In spinal fusion, where the disc is removed and fixed with a metal device, the discs adjacent to the fixed area are more likely to be overloaded after the surgery, which may worsen the spondylolisthesis or cause disc herniation. As part of the rehabilitation on the next day after spinal fusion surgery, patients start moving their leg muscles and performing basic movements such as turning over in bed etc.
During rehabilitation, while following a doctor, nurse, or medical therapist, patients usually exercise the upper body by abdominal breathing / deep breathing, and do lower body exercises such as ankle flexion / extension, leg raising etc. If possible, standing movements are included to prepare the patient for full-scale rehabilitation. Once full-scale rehabilitation begins, patients start to practice walking and other daily activities to get used to postoperative life. In this way, patients are prepared to accept pain through rehabilitation and get ready for their daily life. Therefore, the disadvantage of spinal fusion surgery is that it takes a long time for many patients to return to society after undergoing spinal fusion surgery because they need to undergo rehabilitation. In addition, movement disorders may remain after surgery and it is necessary to avoid movements such as excessive bending, twisting of the waist and back as much as possible.
Potential risks posed by the spinal fusion procedure
The surgical procedure may damage nerves and blood vessels and may cause bacterial contamination and suppuration in the operated area, resulting in complications and infections.
In the case of a spinal fusion procedure, the lumbar spine may shift in place if damage to the fixation device or some loosening of the screws occur. Alternatively, there is a risk that the patient's exact physical condition may not be asserted correctly prior to the procedure due to poor communication with the doctor beforehand, or an allergic reaction due to metal or artificial components may also occur after the surgery. In addition, attaching a fixation device may cause discomfort, fatigue, and persistent pain in the lower back, with symptoms lasting for as long as a year in some cases. The vertebrae also become permanently immobilized after the operation, which translates into a limited use of the body, so the patient will have to bend and twist at the waist instead, making some movements difficult.
At our hospital, we are providing low back pain treatment, with release from the clinic on the same day, to treat patients whose old age would pose high risks during surgery, or who suffered a relapse of their condition in the wake of their previous surgery.
Alternative treatment to spinal fusion
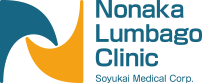
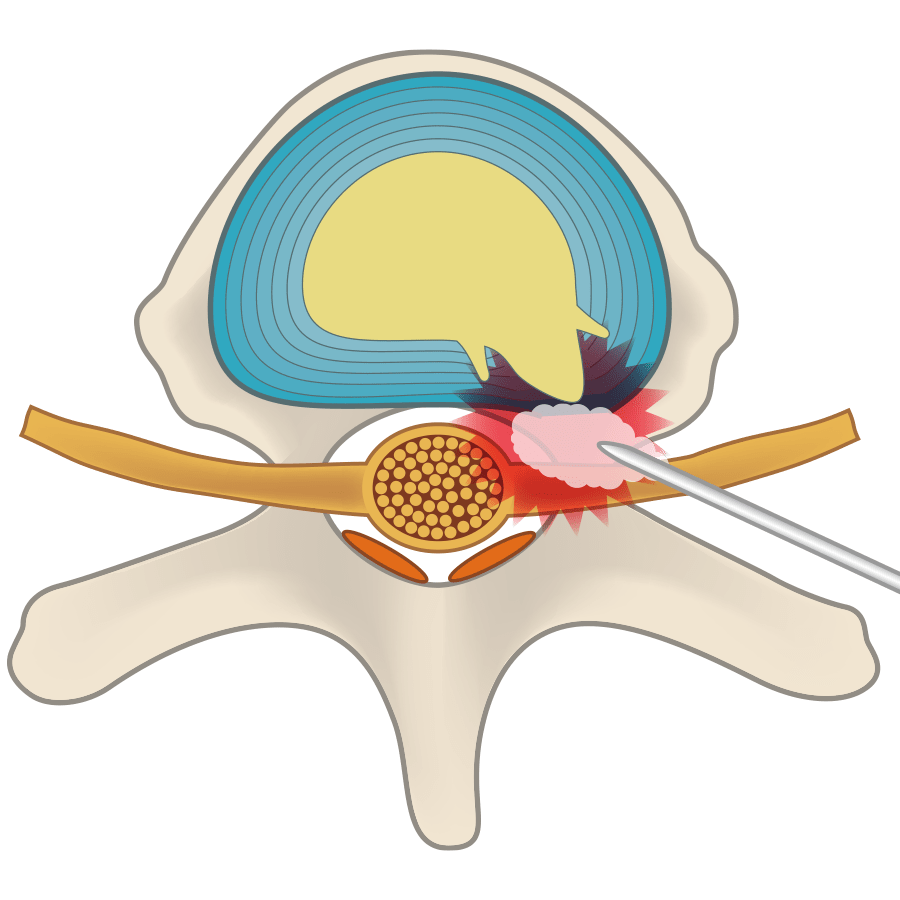
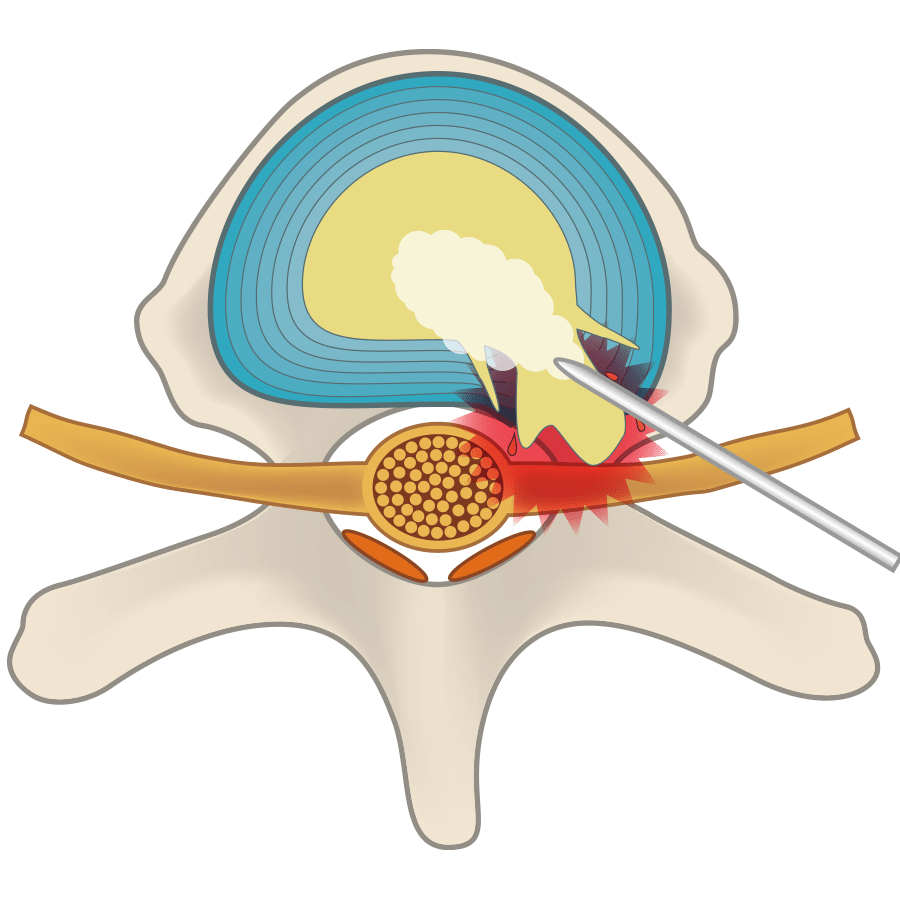
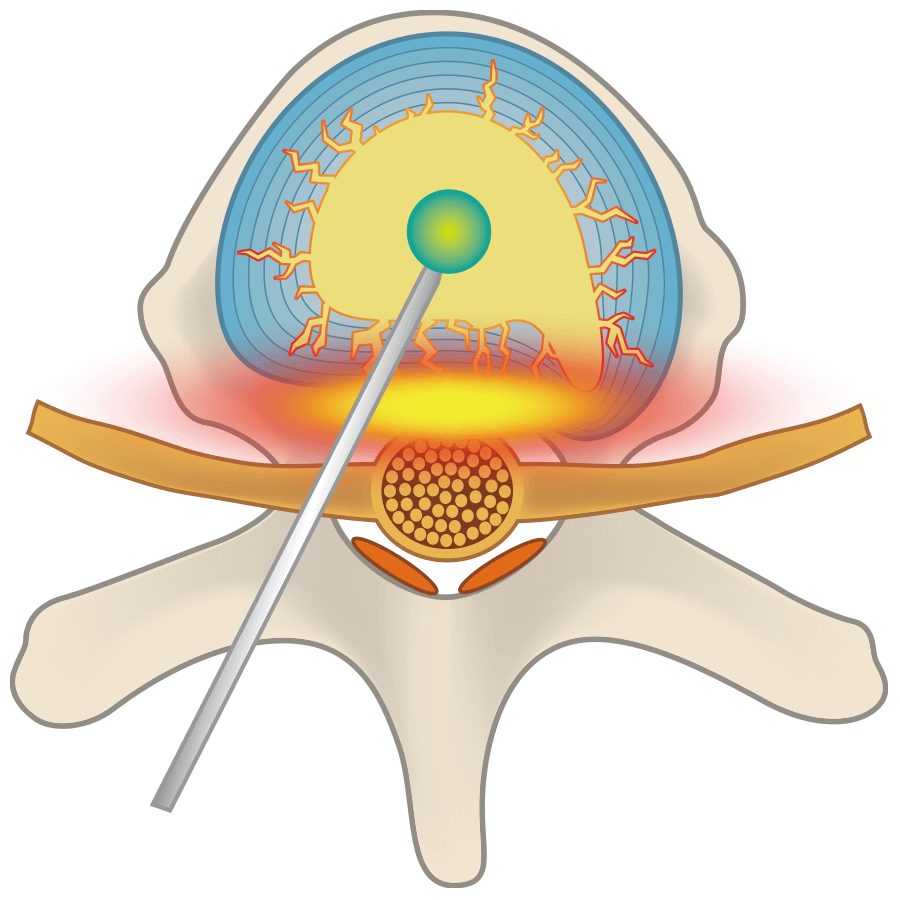
Discseel® Procedure is one of the most effective minimally invasive treatment procedures provided in our clinic as an alternative to spinal fusion. This regenerative spine procedure is used mainly as a treatment option for lumbar disc herniation, lumbar spinal canal stenosis, lumbar spondylolisthesis, lumbar degenerative spondylolisthesis, disc degeneration, and lumbar instability. Since the intervertebral disc is approached with a single needle, there is no need to make any incisions and unnecessary damage to the bones ligaments and surrounding tissues is avoided. The treatment involves injecting a medicine into the cracked disc that repairs it and allows it to regenerate. Repairing the damaged disc prevents the nucleus pulposus from leaking and as a result the inflammation that causes pain and numbness disappears. Hospitalization is not necessary, so patients can return home within the same day after the treatment. Being a minimally invasive outpatient procedure, Discseel® Procedure is less physically demanding which makes it suitable for elderly high-risk surgical patients or patients who experience pain and numbness after undergoing a spinal fusion surgery.
The Discseel® Procedure
Spinal Fusion
Differences between the Discseel® Procedure and Spinal Fusion

Duration of treatment
Spinal fusion is performed under general anesthesia, and a scalpel is used to make a skin incision to remove the vertebral arch, spinous process, and intervertebral joints in the back. The surgery takes approximatively 2 hours. The Discseel® Procedure is performed using a thin needle after local anesthesia. This method of treatment puts less strain on the body since no incision is required, the wound is small and minimally invasive, and the operation time is minimal (as short as 25 minutes).

Risks inherent to the treatment
The skin incision made with a scalpel has the average length of 15 cm and may carry a risk of postoperative complications and infection. In addition, spinal fusion surgery may cause nerve damage and metal allergic reactions to the fixation device. The Discseel® Procedure does not involve any skin incision, but instead uses a needle for treatment, which results in a small dermal puncture of approximately 1.0 to 0.8 mm, so it is less likely to cause nerve damage and has a very low risk of infection and complications.

Recurrence rate
The recurrence rate for spinal fusion surgery is said to be between 30 and 45% (*1). Many patients also undergo revision surgery. The Discseel® Procedure repairs the disc and prevents the nucleus pulposus from leaking through the disc, so the recurrence rate is extremely low.

Going back to narmal life
If you undergo a spinal fusion, you will need to stay in the hospital for about two weeks and take rehabilitation sessions for about a month. No hospitalization is needed for our method of treatment, simply the patient must rest in bed for approximately an hour after the after Discseel® Procedure is performed. The patient can then go home on the same day and is able to do desk work on the following day.
1 "Pain Medicine 12. Review article failed back syndrome," 2011.
British Journal of Pain6. "Whose failure Time to discard a redundant term. 2012
Tatsuro Yamamoto, Keiichi Omote, Tatsuro Yamamoto, Masako Izeki, and Kihito Kawamada: “The Science of Low Back Pain”, Kobundo, May 2014.
Multiple research reviews referenced
Discseel® Procedure and Spine Fusion Surgical Risk Comparison
Please swipe to view ⇒
| The Discseel® Procedure | Spine Fusion | |
|---|---|---|
| Operative time | Approximately 25 minutes | Approximately 2-3 hours |
| Surgical bleeding | Low | High |
| Risk of complications | Low | High |
| Hospitalization period | None | Approximately 3 weeks |
| Recurrence rate within 2 years after surgery |
Low | High |
| Postoperative restrictions | Daily life is possible from the next day | Approximately 1 month is needed to return to daily life activities |
If you are about to undergo a spinal fusion surgery, please make sure you carefully listen to the explanations prior to it and fully understand the the risks involved. After spinal fusion, the fixed lumbar vertebrae becomes immobile, making it easier to overload the adjacent discs. As a result, the intervertebral discs can degenerate, causing conditions such as spondylolisthesis and disc herniation etc. The risk of developing adjacent intervertebral disorders increases with the number of fixed vertebrae. In contrast to these surgical methods, our clinic uses the Discseel® Procedure, which is less stressful to the body and can be performed on an outpatient basis.
Frequently Asked Questions
-
- Q
-
I have been experiencing pain and numbness for quite a long time now. Should I see a doctor?
- A
-
If the pain or numbness persists for more than a month, we recommend that you consult a doctor. X-rays and MRIs will be performed to determine the cause of the pain and numbness, and a diagnosis will be made.
-
- Q
-
Is it possible to treat spondylolisthesis using The Discseel® Procedure?
- A
-
We can also treat spondylolisthesis if the procedure is deemed suitable for your pathology. Please contact us for a consultation so that we can determine if you are eligible for treatment.
-
- Q
-
I am experiencing continuous pain and numbness after undergoing spinal fusion surgery previously. Is there any way to improve my condition?
- A
-
If lumbar disc herniation, lumbar spinal canal stenosis, lumbar spondylolisthesis, or a lumbar degenerative spondylolisthesis are confirmed, conservative treatments will usually be performed according to the doctor's instructions. Or, The Discseel® Procedure can also be applied as a minimally invasive treatment alternative to spinal fusions that cannot be re-operated.
-
- Q
-
Is The Discseel® Procedure only available at the NLC Nonaka Lumbago Clinic?
- A
-
Yes, we are currently the only hospital in Japan that is fully accredited to perform The Discseel® Procedure. In addition to being a minimally invasive treatment, we also provide a one-day treatment.
-
- Q
-
Should I continue rehabilitation after leaving the hospital?
- A
-
Yes, it is important to continue rehabilitation to prevent recurrence of the pathology. It is necessary to avoid heavy labor as much as possible and try to perform movements without putting a strain on your lower back. If you are experiencing severe pain or numbness, you should consult with a doctor to discuss the appropriate exercises. Since we are operating in coordination with a rehabilitation facility, we can also provide exercise guidance and training.
-
- Q
-
Does spinal fusion leave any kind of mobility problems?
- A
-
After the surgery, the patient may experience some temporary mobility problems due to the loss of motor functions, but this will gradually be alleviated with about a month of rehabilitation after the surgery. However, elderly patients or those who have suffered complications, may be left with movement disorder, so you should check and be aware of the postoperative risk before undergoing spinal fusion surgery.
-
- Q
-
What causes adjacent intervertebral disorders after spinal fusion? Also, is there any way to deal with the adjacent intervertebral disorder if it has occurred?
- A
-
Adjacent intervertebral disc disorder is damage or deformation of the intervertebral discs adjacent to the intervertebral vertebrae that have undergone spinal fusion surgery. When it worsens, it may lead to diseases such as disc herniation, spinal canal stenosis, and spondylolisthesis. If the symptoms of adjacent disc damage are mild, corsets, rehabilitation and medication may be the treatment of choice, but if the symptoms are severe, surgery may be considered. If symptoms are caused by disc herniation, a discectomy called PED/PELD may be performed, and if the cause is spondylolisthesis, spinal fusion may be selected as the treatment of choice. The Discseel® Procedure also is also a treatment that can be applied after spinal fusion surgery. It is designed to repair and regenerate disc deformation without causing the symptoms of adjacent disc disorder to worsen.
-
- Q
-
Is there a possibility of complications after spinal fusion surgery?
- A
-
Yes, there is a possibility of complications. In spinal fusion, a scalpel is used to make an incision, which puts a heavy burden on the body and poses a risk of postoperative complications. The Discseel® Procedure and some other disc treatment methods available at our clinic do not use scalpels, and are performed with thin needles, so there is less risk of complications and less burden on the patient's body compared to spinal fusion.
Treatment Overview
The Discseel
Discseel® Procedure
Discseel® Procedure was developed by an American surgeon by the name of Dr. Kevin Pauza, after caring for hundreds of patients who were made worse following their spine surgery. The treatment aims to seal tears in herniated vertebral discs and help them regenerate and recover their, allowing permanent relief of back pain. Dr. Pauza holds a series of 16 patents for a device and Discseel® biologic that support the treatment. Dr.Nonaka has been licensed to perform the Discseel® Procedure in 2018, and more than 2,880 patient have undergone the treatment in our clinic since then. At present, approximately 20 doctors, including physicians from Harvard and Boston Universities are using the Discseel® Procedure to treat their patients in the USA. Dr. Nonaka is the first physician trained to perform the Discseel® Procedure in Japan.
-
The PLOT Method
(Laser And Ozone)Percutaneous Laser and Ozone Treatment

-
The PODT Method
(Ozone)Percutaneous Ozone Disc
Treatment
-
The PLDD Method
(Laser)Percutaneous Laser Disc
Decompression
Targeted Conditions
-
Disc Herniation

-
Spinal Canal Stenosis

-
Sciatica

-
Spondylolisthesis

-
Disc Degeneration

-
Lumbar Spondylosis

- HOME/
- Targeted Conditions/
- Alternative treatments to spinal fusion